What is Cartilage Autograft?
Cartilage autograft (also called osteochondral autograft transfer or OATS) is an arthroscopic surgical procedure performed to replace damaged articular cartilage of the knee with a patient’s own healthy bone and cartilage (autograft).
Key statistics about Cartilage Autograft
- Approximately 12% of the population suffer from cartilage defects in the knee[1]
- 60% of patients who undergo knee arthroscopy are discovered to have cartilage defects[2]
- Approximately 72% of patients who undergo cartilage autograft have successful outcomes up to 10 years after the procedure[3]
Expert Insights
The Goals of Treating Cartilage Injuries - Daniel Cooper, MD
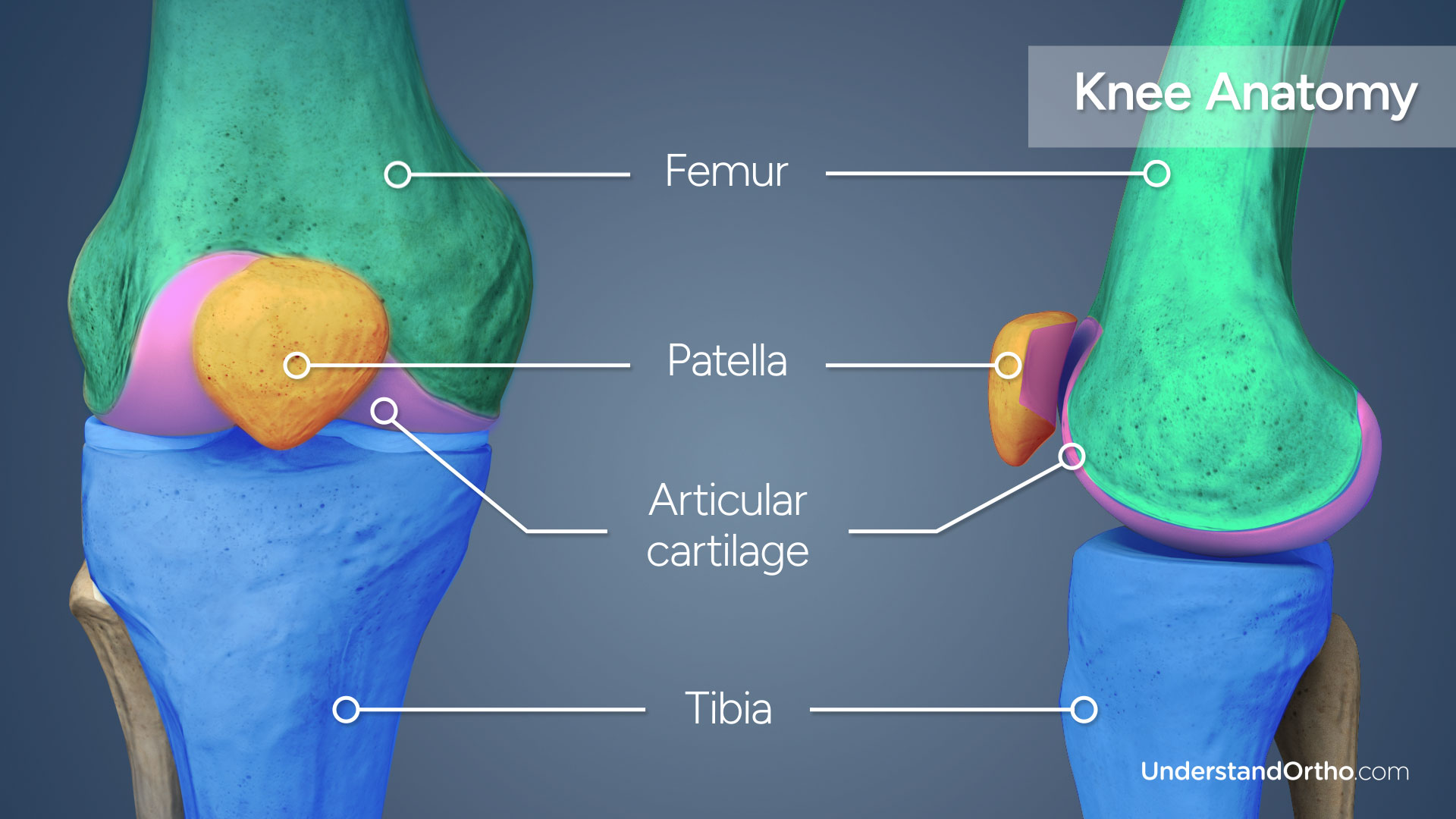
Knee Anatomy
The knee joint is formed by three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap).
Articular cartilage covers the ends of the bones, helping with shock absorption and allowing the bones to glide smoothly against one another. Articular cartilage is made up of cells called chondrocytes.
Why is Cartilage Autograft performed?
Articular cartilage damage can expose the underlying bone, causing pain and affecting joint function as the knee moves. Cartilage autograft is performed to address cartilage injuries to the knee joint in order to alleviate pain and restore a smooth joint surface. This procedure can also prevent the progression of cartilage damage and delay knee replacement.
Cartilage autograft removes a patient’s own healthy bone and cartilage and transplants it to the damaged area of articular cartilage, repairing the injury. If the bone and cartilage damage is too extensive, a cartilage allograft using bone and cartilage from a human donor may be used instead.
Who needs Cartilage Autograft?
Damage to articular cartilage of the knee typically is caused by overuse or injury.
Ideal candidates for the procedure have smaller regions of cartilage damage (no widespread osteoarthritis or rheumatoid arthritis), have normal knee alignment and stability, and are relatively young, active, and willing to commit to physical therapy.
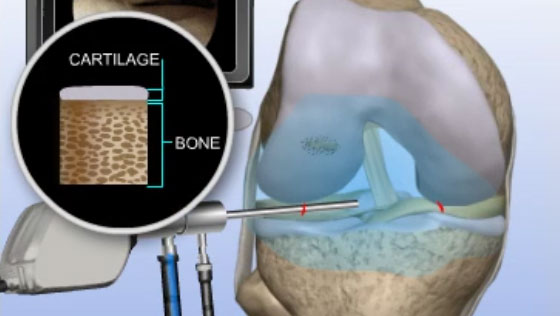
How is Cartilage Autograft performed?
- The surgeon will make small incisions around the knee joint and the arthroscope will be inserted into one of the incisions.
- Saline solution is pumped into the joint to expand it and improve visualization.
- Images from the arthroscope are sent to a video monitor where the surgeon can see inside the joint.
- Healthy bone and cartilage is harvested from a low weight-bearing area of your femur.
- Any damaged tissue is removed from the injured cartilage and the surrounding area is smoothed.
- The healthy tissue is inserted into the region of injured cartilage and if necessary, additional healthy tissue may be harvested and inserted to completely fill the damaged area.
- Finally, the saline solution is drained, instruments are removed, and the incisions are closed using sutures.
What are the risks of Cartilage Autograft?
Risks associated with cartilage autograft may include:
- Infection
- Blood clots
- Nerve or blood vessel damage
- Persistent knee swelling
- Graft failure
- Bleeding and pain at the donor site
How long does it take to recover from Cartilage Autograft?
-
24 hours after surgery
Most patients are able to return home the same day as their procedure. A physical therapy routine will be established by the surgeon and physical therapist, and pain medication may be prescribed. Crutches will be provided to keep weight off the affected leg. -
2 weeks after surgery
Any non-dissolvable sutures are removed and bruising and swelling begin to subside. -
4-6 weeks after surgery
Most patients can walk with full weight on the affected leg and resume most daily activities. -
6-9 months after surgery
Most patients are fully recovered from cartilage autograft.
What are the results of Cartilage Autograft?
Cartilage autograft is a safe and effective procedure performed to treat mild to moderate areas of articular cartilage damage within the knee joint. For patients who meet eligibility criteria for the procedure, this treatment can provide significant improvement in knee function and persistent pain.
Find an Orthopedic Doctor in Your Area