What is Reverse Total Shoulder Replacement?
Reverse total shoulder replacement (also known as RTSR, reverse total shoulder arthroplasty, or RTSA) is a surgical procedure performed to replace damaged portions of the shoulder joint with an artificial implant. While a conventional total shoulder replacement implant resembles typical shoulder anatomy, a reverse total shoulder replacement implant reverses the ball and socket of the joint.
Key statistics about Reverse Total Shoulder Replacement
- Nearly 825,000 individuals in the United States are living with a shoulder replacement[1]
- More than 60,000 reverse total shoulder replacement procedures are performed in the United States each year[2]
- 92% of patients who undergo reverse total shoulder replacement report their shoulder function as “better” or “much better”[3]
- 93% of reverse total shoulder replacement implants will last 10 years[4]
Expert Insights
What to Expect from Total Shoulder Replacement - Jason Klein, MD
Shoulder Anatomy
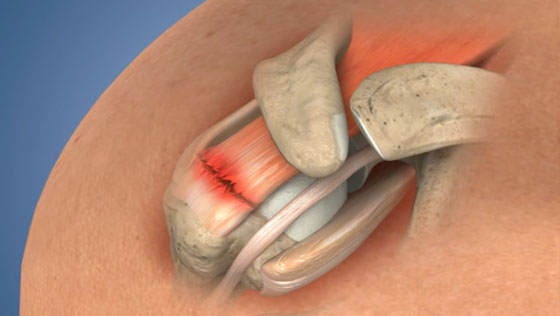
The shoulder is a ball-and-socket joint formed by three bones: the humerus, the scapula, and the clavicle. The head of the humerus rests in the socket of the scapula, also called the glenoid.

The rotator cuff is made up of a group of four tendons and muscles that surround the shoulder joint. These muscles are the subscapularis, the supraspinatus, the infraspinatus, and the teres minor, and together they work to stabilize the joint and move the arm.

Why is Total Shoulder Replacement performed?
Reverse total shoulder replacement is performed primarily to relieve pain and joint dysfunction caused by arthritis and severe rotator cuff damage. Rotator cuff arthropathy is a degenerative condition that arises after severe damage to the rotator cuff causes malalignment in the shoulder joint, leading to arthritis. Arthritis occurs as the cartilage that cushions the shoulder wears down, causing the bones to grind against each other. This results in pain and inflammation, and can lead to bone deformity and a loss of joint mobility.

When the cartilage damage from arthritis is so severe that all cartilage must be removed, a shoulder replacement is performed. There are two types of total shoulder replacement surgery:
- Conventional (anatomic) total shoulder replacement: in which the implant resembles the typical ball-in-socket shoulder joint anatomy
- Reverse total shoulder replacement: in which the implant reverses typical shoulder joint anatomy, with the ball being placed on the shoulder socket and the stem replacing the head of the humerus
The determination between which surgery should be performed is based upon the strength and functionality of the rotator cuff. A reverse total shoulder replacement configuration depends on the deltoid muscle instead of the rotator cuff to stabilize the shoulder and provide joint mobility and is often a better option for patients who have severe rotator cuff damage.

Who needs Reverse Total Shoulder Replacement?
Reverse total shoulder replacement typically is recommended for patients who suffer from rotator cuff arthropathy due to rotator cuff damage from a traumatic injury or from a prior untreated rotator cuff tear. Additionally, this procedure may be recommended for individuals who have undergone previously unsuccessful conventional total shoulder replacement surgery.
How is Reverse Total Shoulder Replacement performed?
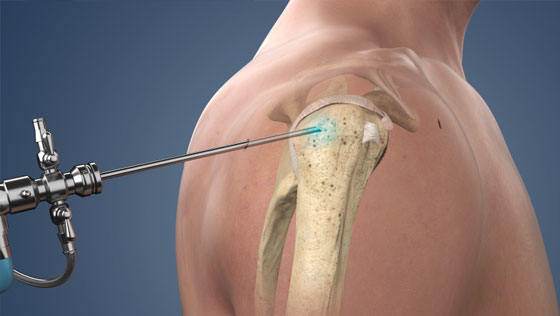
- The surgeon will make an incision and access the shoulder joint.
- The head of the humerus is removed.
- The surgeon will insert the humeral stem implant into the humerus and fit the plastic cup on the humeral side.
- The glenoid surface is cleaned and prepared for the implant.
- The first portion of the glenoid implant is secured to the bone with screws and the ball portion of the implant is affixed.
- The arm is rotated to place the ball into the socket.
- Finally, the incision will be closed with sutures or surgical staples.

What are the risks of Reverse Total Shoulder Replacement?
Potential risks associated with reverse total shoulder replacement may include:
- Infection
- Blood clots
- Nerve or blood vessel damage
- Joint instability
- Joint stiffness
- Bone fracture around the implant
- Loosening or wearing down of the implant over time
How long does it take to recover from Reverse Total Shoulder Replacement?
-
1-3 days after surgery
Most patients are discharged from the hospital. A physical therapy routine will be established by the surgeon and physical therapist, and pain medication may be prescribed. A sling will be provided, but it is important that prescribed exercises are followed in order to prevent the development of any weakness or stiffness. -
2 weeks after surgery
Any non-dissolvable sutures and staples are removed and bruising and swelling begin to subside. -
6-8 weeks after surgery
Most patients are able to discontinue use of the sling and resume most daily activity. -
6 months after surgery
Most patients report being pain-free, but it may take some patients up to 12 months to fully recover from reverse total shoulder replacement.
What are the results of Reverse Total Shoulder Replacement?
Reverse total shoulder replacement alleviates pain and restores shoulder function for patients with severe rotator cuff damage and shoulder arthritis, and the surgery has a high degree of patient satisfaction. 92% of patients who undergo reverse total shoulder replacement report their shoulder function as “”better” or “much better.”[3]
Find an Orthopedic Doctor in Your Area