Damaged Patellar Cartilage Removal
Patellar cartilage removal (also known as cartilage debridement or chondroplasty) is an arthroscopic surgical procedure performed to remove damaged articular cartilage behind the patella.
Key statistics about Damaged Patellar Cartilage Removal
- Approximately 12% of the population suffer from cartilage defects in the knee[1]
- 60% of patients who undergo knee arthroscopy are discovered to have cartilage defects[2]
Knee Anatomy
The knee joint is formed by three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). As the knee bends and straightens, the patella moves back and forth within a groove on the femur called the trochlea.

Articular cartilage covers the ends of the femur and tibia, the trochlea, and the underside of the patella, helping with shock absorption and allowing the bones to glide smoothly against one another.

Why is Patellar Cartilage Removal performed?
Articular cartilage damage can cause pain and affect knee joint function. If the damage is significant enough, the cartilage injuries can be surgically removed within the knee joint (Damaged Knee Articular Cartilage Removal) or behind the patella.
The goal of patellar cartilage removal is to address cartilage injuries of the patella and trochlea in order to alleviate pain and restore a smooth joint surface. This procedure can also prevent the progression of cartilage damage and delay knee replacement.
Who needs Patellar Cartilage Removal?
Damage to patellar articular cartilage typically is caused by overuse or injury.
Ideal candidates for the procedure have smaller regions of patellar cartilage damage (no widespread osteoarthritis or rheumatoid arthritis), have normal knee alignment and stability, and are relatively young, active, and willing to commit to physical therapy.
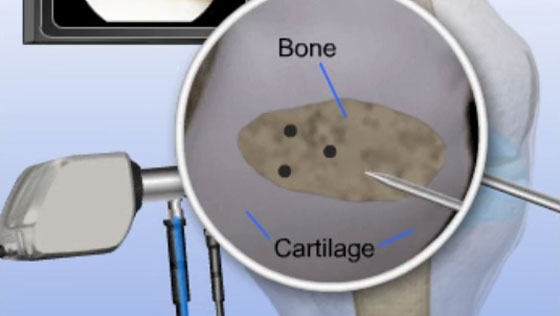
How is Patellar Cartilage Removal performed?
- The surgeon will make small incisions around the knee joint and the arthroscope will be inserted into one of the incisions.
- Saline solution is pumped into the joint to expand it and improve visualization.
- Images from the arthroscope are sent to a video monitor where the surgeon can see inside the joint.
- The damaged cartilage on the underside of the patella is removed.
- The surgeon may choose to scrape the exposed bone in order to stimulate healing.
- Finally, the saline solution is drained, instruments are removed, and the incisions are closed using sutures.
What are the risks of Patellar Cartilage removal?
It is uncommon to experience complications from patellar cartilage removal but potential risks may include:
- Infection
- Blood clots
- Nerve or blood vessel damage
- Knee stiffness
How long does it take to recover from Patellar Cartilage Removal?
-
24 hours after surgery
Most patients are able to return home the same day as their procedure. A physical therapy routine will be established by the surgeon and physical therapist, and crutches will be provided. Pain medication may be prescribed. -
2 weeks after surgery
Any non-dissolvable sutures are removed and bruising and swelling begin to subside. -
4-7 months after surgery
Most patients are able to resume daily activities, including walking without assistance. -
9-12 months after surgery
Most patients are fully recovered from microfracture surgery.
What are the results of Patellar Cartilage Removal?
Patellar cartilage removal is a safe and effective procedure performed to treat mild to moderate areas of articular cartilage damage behind the patella. For patients who meet eligibility criteria for cartilage removal, the surgery can provide significant improvement in knee function and persistent pain.
Find an Orthopedic Doctor in Your Area